Juvenile Hallux Abducto Valgus Deformity
Overview
 Bunions are the most common deformity that affects the big toe. A bunion is characterized by angling of the big toe towards the lesser toes, and a painful bump over the inside part of the base of the big toe. This prominence (an area called the medial eminence) is caused by angling inwards of the metatarsal bone, and is not an actual growth of bone.
Bunions are the most common deformity that affects the big toe. A bunion is characterized by angling of the big toe towards the lesser toes, and a painful bump over the inside part of the base of the big toe. This prominence (an area called the medial eminence) is caused by angling inwards of the metatarsal bone, and is not an actual growth of bone.
Causes
Bunions are caused by pressure on the inside of the forefoot which causes the 1st metatarsal bone in the foot to migrating outwards. Biomechanical factors can contribute to the development of bunions for example if you over pronate where the foot rolls in or flattens excessively which causes the inside of the foot to rub against the shoe. Wearing high heeled shoes regularly also increases the risk of developing the condition . The pressure on the forefoot is increased considerably as the heel is raised up. Age is also a factor as the ligaments lose strength as you get older.
Symptoms
Since the pain from a bunion is always aggravated by shoe wear, the symptoms will often depend on the type and size of shoes worn. The perception of pain or discomfort that people experience is quite varied. There are some individuals who have small bunions that are very uncomfortable. This limits their ability to wear shoes comfortably. On the other hand, some individuals may have quite significant deformities that are annoying but do not limit their activities in anyway.
Diagnosis
Looking at the problem area on the foot is the best way to discover a bunion. If it has the shape characteristic of a bunion, this is the first hint of a problem. The doctor may also look at the shape of your leg, ankle, and foot while you are standing, and check the range of motion of your toe and joints by asking you to move your toes in different directions A closer examination with weight-bearing X-rays helps your doctor examine the actual bone structure at the joint and see how severe the problem is. A doctor may ask about the types of shoes you wear, sports or activities (e.g., ballet) you participate in, and whether or not you have had a recent injury. This information will help determine your treatment.
Non Surgical Treatment
In the early stages of the formation of a bunion, soaking feet in warm water can provide temporary relief. The best way to alleviate the pain associated with bunions is to wear properly fitting shoes. Shoes designed with a high, wide toe box (toe area) are recommended for people suffering from forefoot disorders, such as bunions. Shoes with rocker soles will unload pressure to the bunion area. Orthotics are also recommended for this condition to provide extra comfort, support, and protection. Other conservative treatments include using forefoot products designed to accommodate and relieve bunions such as bunion shields, bunion night splints, and bunion bandages. These conservative treatments can limit the progression of the bunion formation, relieve pain and provide a healthy environment for the foot. 
Surgical Treatment
When deciding whether to have bunion surgery, there are several things to consider including your age, in children, bunion surgery is often delayed because of the risk of the bunion returning, your medical history and general health, problems with wound healing and infections are more likely in certain conditions such as diabetes, you?re also more likely to develop problems if your bunion is caused by a condition such as rheumatoid arthritis, your occupation and lifestyle, bunion surgery can make your toes less flexible, and you may be unable to return to the same level of physical activity, your expectations of surgery, bunion surgery has about an 85% success rate, but there's no guarantee that your foot will be perfectly straight or pain-free; the success of surgery depends on the type of procedure, the experience of the surgeon and your ability to rest after the operation, the severity of your symptoms, surgery will usually only be recommended if your bunions are causing considerable pain and non-surgical treatments haven't been unsuccessful (because of the associated risks and complications).
Will Over-Pronation Of The Feet Have To Have Surgery
While a slight amount of pronation is the proper means to absorb shock naturally, too much pronation (over-pronation) can potentially contribute to many maladies, which can sideline a runner. A foot that pronates excessively is one that continues to roll inward past a neutral position after the shock of impact has been absorbed. Uncorrected and repeated, this motion may lead to repetitive stress related injuries of the feet and legs. More times than not, the runner who over-pronates needs a shoe that reduces excess pronation and guides the foot along a neutral path.

Causes
Over-pronation may happen because the tissue that attaches to your foot bones is loose. You may be born with this problem or it may result from injuries or overuse, like from too much running.
Symptoms
If you overpronate, your symptoms may include discomfort in the arch and sole of foot, your foot may appear to turn outward at the ankle, your shoes wear down faster on the medial (inner) side of your shoes. Pain in ankle, shins, knees, or hips, especially when walking or running are classic symptoms of overpronation. Overpronation can lead to additional problems with your feet, ankles, and knees. Runners in particular find that overpronation can lead to shin splints, tarsal tunnel syndrome, plantar fasciitis, compartment syndrome, achilles tendonitis, bunions or hallux valgus, patello-femoral pain syndrome, heel spurs, metatarsalgia.
Diagnosis
To easily get an idea of whether a person overpronates, look at the position and condition of certain structures in the feet and ankles when he/she stands still. When performing weight-bearing activities like walking or running, muscles and other soft tissue structures work to control gravity's effect and ground reaction forces to the joints. If the muscles of the leg, pelvis, and feet are working correctly, then the joints in these areas such as the knees, hips, and ankles will experience less stress. However, if the muscles and other soft tissues are not working efficiently, then structural changes and clues in the feet are visible and indicate habitual overpronation.
Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improper fitting footwear can lead to additional problems of the foot. If the problem persists, call your doctor to schedule an appointment.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
What Would Cause Severs Disease?
Sever's disease is a common cause of heel pain, particularly in the young and physically active. During puberty the calcaneus consist of two areas of bone known as ossification centres. These two areas are divided by an area of cartilage known as the calcaneal apophysitis. See x-ray (right) for two ossification centres of heel. The Achilles tendon attaches the triceps surae (calf muscles) to the calcaneus (heel bone). As a child grows the calcaneus grow faster than the surrounding soft tissue, which means the Achilles tendon is pulled uncomfortably tight. This increase in tensile load can cause inflammation and irritation of the calcaneal apophysis (growth plate) which is known as Sever's Disease. The pain is exacerbated by physical activities, especially ones involving running or jumping. Sever's disease most commonly affects boys aged 12 to 14 years and girls aged 10 to 12 years, which corresponds with the early growth spurts of puberty.
Causes
Sever?s disease only occurs during a certain period of pre-adolescence, when the heel bone is going through a rapid growth spurt. In girls, this typically occurs around 8 to 10 years of age, and in boys, between ages 10 and 13. Sever?s disease is more common in active, athletic children. The condition is difficult to prevent completely, but changing the type and amount of physical activity when your child is experiencing pain will help.
Symptoms
Some of the most common signs and symptoms associated with Sever?s disease include. Heel pain or tenderness in one or both heels, usually at the back of the heel. Pain or discomfort upon waking, or when the heel is squeezed. Heel pain that is worse during or following activity. Limping. Heel swelling or redness. Tight calf muscles. Decreased ankle range of motion.
Diagnosis
A doctor can usually tell that a child has Sever's disease based on the symptoms reported. To confirm the diagnosis, the doctor will probably examine the heels and ask about the child's activity level and participation in sports. The doctor might also use the squeeze test, squeezing the back part of the heel from both sides at the same time to see if doing so causes pain. The doctor might also ask the child to stand on tiptoes to see if that position causes pain. Although imaging tests such as X-rays generally are not that helpful in diagnosing Sever's disease, some doctors order them to rule out other problems, such as fractures. Sever's disease cannot be seen on an X-ray.
Non Surgical Treatment
Sever?s disease treatment should be based on eliminating pain and restoring normal foot and leg biomechanics. As with most soft tissue injuries the initial treatment is Rest, Ice, and Protect. In the early phase you?ll most likely be unable to walk pain-free. Our first aim is to provide you with some active rest from pain-provoking activities. "No Pain. No Gain." does not apply in Sever's disease. If it hurts your child is doing too much exercise. Your child should reduce or cease any activity that causes heel pain. Ice is a simple and effective modality to reduce your pain and swelling. Please apply for 20-30 minutes each 2 to 4 hours during the initial phase or when you notice that your injury is warm or hot. Most children can tolerate paracetamol as a pain reducing medication. Check with your doctor. To support and protect your heels, you may need to be wear shock absorbing heel cups or a soft orthotic. Kinesio foot taping may help to provide pain relief.
Recovery
With proper care, your child should feel better within 2 weeks to 2 months. Your child can start playing sports again only when the heel pain is gone. Your doctor will let you know when physical activity is safe.
Achilles Tendon Repair Cast Aluminum
Overview
 Achilles tendon ruptures commonly occur in athletic individuals in their 30s and 40s while performing activities that require sudden acceleration or changes in direction (ex. basketball, tennis, etc.). Patients usually describe a sharp pain in their heel region almost as if they were ?struck in the back of the leg?. The diagnosis of an acute Achilles tendon rupture is made on clinical examination as x-rays will reveal the ankle bones to be normal. The Achilles is the largest and strongest tendon in the body. It is subject to 2-3 times body weight during normal walking so regaining normal Achilles tendon function is critical. Achilles tendon ruptures can be successfully treated non-operatively, or operatively, but they must be treated. Surgical treatment leads to a faster recovery and a lower rate of re-rupture. However, surgery can be associated with very serious complications such as an infection or wound healing problems. For this reason non-operative treatment may be preferable in many individuals, especially those patients with diabetes, vascular disease, and those who are long-term smokers.
Achilles tendon ruptures commonly occur in athletic individuals in their 30s and 40s while performing activities that require sudden acceleration or changes in direction (ex. basketball, tennis, etc.). Patients usually describe a sharp pain in their heel region almost as if they were ?struck in the back of the leg?. The diagnosis of an acute Achilles tendon rupture is made on clinical examination as x-rays will reveal the ankle bones to be normal. The Achilles is the largest and strongest tendon in the body. It is subject to 2-3 times body weight during normal walking so regaining normal Achilles tendon function is critical. Achilles tendon ruptures can be successfully treated non-operatively, or operatively, but they must be treated. Surgical treatment leads to a faster recovery and a lower rate of re-rupture. However, surgery can be associated with very serious complications such as an infection or wound healing problems. For this reason non-operative treatment may be preferable in many individuals, especially those patients with diabetes, vascular disease, and those who are long-term smokers.
Causes
Causes of and contributors to Achilles tendon rupture include trauma (caused by injury, usually an acceleration injury such as pushing off or jumping up). Preceding tendon problems. Chronic Achilles tendonitis (can lead to small tears within the tendon, increasingly weakening it). Certain drug therapies/treatments. Drugs that have been linked to Achilles tendon rupture include. Fluoroquinolone antibiotics - after nearly 900 reports of tendon ruptures, tendonitis and other tendon disorders (most associated with the Achilles tendon) linked to Ciprofloxacin (Cipro) alone were collected in the U.S. Food and Drug Administration (FDA)?s database, at least one public-interest group petitioned the FDA to recommend that a "Black Box Warning" be added to Cipro's packaging. Some researchers speculate this class of antibiotics is toxic to tendon fibers, and that in some cases may reduce their blood supply. Patients should at least be more aware of the potential for ruptures so that they can be switched to other antibiotics at the onset of early warning signals such as tendon pain.
Symptoms
Symptoms of an Achilles tendon injury are as follows. Pain along the back of your foot and above your heel, especially when stretching your ankle or standing on your toes; with tendinitis, pain may be mild and worsen gradually. If you rupture the tendon, pain can be abrupt and severe. Tenderness. Swelling. Stiffness. Hearing a snapping or popping noise during the injury. Difficulty flexing your foot or pointing your toes (in complete tears of the tendon).
Diagnosis
Your doctor will ask you about your symptoms and examine you. He or she may also ask you about your medical history. Your doctor may ask you to do a series of movements or exercises to see how well you can move your lower leg. He or she may also examine your leg, heel and ankle and may squeeze your calf muscle to check the movement of your foot. You may need to have further tests to confirm if your tendon is torn, which may include the following. An ultrasound scan. This uses sound waves to produce an image of the inside of your leg. An MRI scan. This uses magnets and radio waves to produce images of the inside of your leg.
Non Surgical Treatment
You may need to wear a plaster cast, brace or boot on your lower leg for six to eight weeks to help the tendon heal. During this time, your doctor will change the cast a number of times to make sure your tendon heals in the right way. If your tendon is partially ruptured, your doctor will probably advise you to have this treatment instead of surgery. It?s also suitable for people who aren't very physically active. However, there is a greater risk that your tendon will rupture again, compared with surgery. Your doctor will advise you which treatment is best for you. 
Surgical Treatment
There are two different types of surgeries; open surgery and percutaneous surgery. During an open surgery an incision is made in the back of the leg and the Achilles tendon is stitched together. In a complete or serious rupture the tendon of plantaris or another vestigial muscle is harvested and wrapped around the Achilles tendon, increasing the strength of the repaired tendon. If the tissue quality is poor, e.g. the injury has been neglected, the surgeon might use a reinforcement mesh (collagen, Artelon or other degradable material). In percutaneous surgery, the surgeon makes several small incisions, rather than one large incision, and sews the tendon back together through the incision(s). Surgery may be delayed for about a week after the rupture to let the swelling go down. For sedentary patients and those who have vasculopathy or risks for poor healing, percutaneous surgical repair may be a better treatment choice than open surgical repair.
Functional Leg Length Discrepancy Description
The type of surgery depends on the type of problem. Outpatient procedures may be used to alter the growth of the limb. This is often done through small incisions. If an outpatient procedure is done, your child can continue with most regular activities. Other times, surgery may be very involved and require the use of an external device that is attached to the limb with pins and wires. This device may be left on for months to correct the deformity or lengthen the leg. If this type of surgery is required, your child will be making weekly visits to Cincinnati Children's.

Causes
Leg length discrepancies can be caused by: hip and knee replacements, lower limb injuries, bone diseases, neuromuscular issues and congenital problems. Although discrepancies of 2 cm or less are most common, discrepancies can be greater than 6 cm. People who have LLD tend to make up for the difference by over bending their longer leg or standing on the toes of their shorter leg. This compensation leads to an inefficient, up and down gait, which is quite tiring and over time can result in posture problems as well as pain in the back, hips, knees and ankles.
Symptoms
The effects of a short leg depend upon the individual and the extent of discrepancy. The most common manifestation if a lateral deviation of the lumbar spine toward the short side with compensatory curves up the spine that can extend into the neck and even impacts the TMJ. Studies have shown that anterior and posterior curve abnormalities also can result.
Diagnosis
The only way to decipher between anatomical and functional leg length inequalities (you can have both) is by a physical measurement and series of biomechanical tests. It is actually a simple process and gets to the true cause of some runner?s chronic foot, knee, hip and back pain. After the muscles are tested and the legs are measured it may be necessary to get a special X-ray that measures both of your thighs (Femurs) and legs (Tibias). The X-ray is read by a medical radiologist who provides a report of the actual difference down to the micrometer leaving zero room for error. Once the difference in leg length is known, the solution becomes clear.
Non Surgical Treatment
In order to measure for correction, use a series of blocks or sheets of firm material (cork or neoprene) of varying thickness, e.g., 1/8", 1/4", and 1/2". Place them under the short limb, either under the heel or the entire foot, depending on the pathology, until the patient feels most balanced. Usually you will not be able to correct for the full amount of the imbalance at the outset. The longer a patient has had the LLD, the less likely he or she will be able to tolerate a full correction immediately. This is a process of incremental improvements. 2 inch External Platform Lift Bear in mind that the initial lift may need to be augmented as the patient's musculoskeletal system begins to adjust. It is often recommended that the initial buildup should be 50 percent of the total. After a suitable break-in period, one month say, another 25 percent can be added. If warranted, the final 25 percent can be added a month later. Once you determine how much lift the patient can handle, you then need to decide how to best apply it. There are certain advantages and disadvantages to using either internal or external heel lifts.

Surgical Treatment
Limb deformity or leg length problems can be treated by applying an external frame to the leg. The frame consists of metal rings which go round the limb. The rings are held onto the body by wires and metal pins which pass through the skin and are anchored into the bone. During this operation, the bone is divided. Gradual adjustment of the frame results in creation of a new bone allowing a limb to be lengthened. The procedure involves the child having an anaesthetic. The child is normally in hospital for one week. The child and family are encouraged to clean pin sites around the limb. The adjustments of the frame (distractions) are performed by the child and/or family. The child is normally encouraged to walk on the operated limb and to actively exercise the joints above and below the frame. The child is normally reviewed on a weekly basis in clinic to monitor the correction of the deformity. The frame normally remains in place for 3 months up to one year depending on the condition which is being treated. The frame is normally removed under a general anaesthetic at the end of treatment.
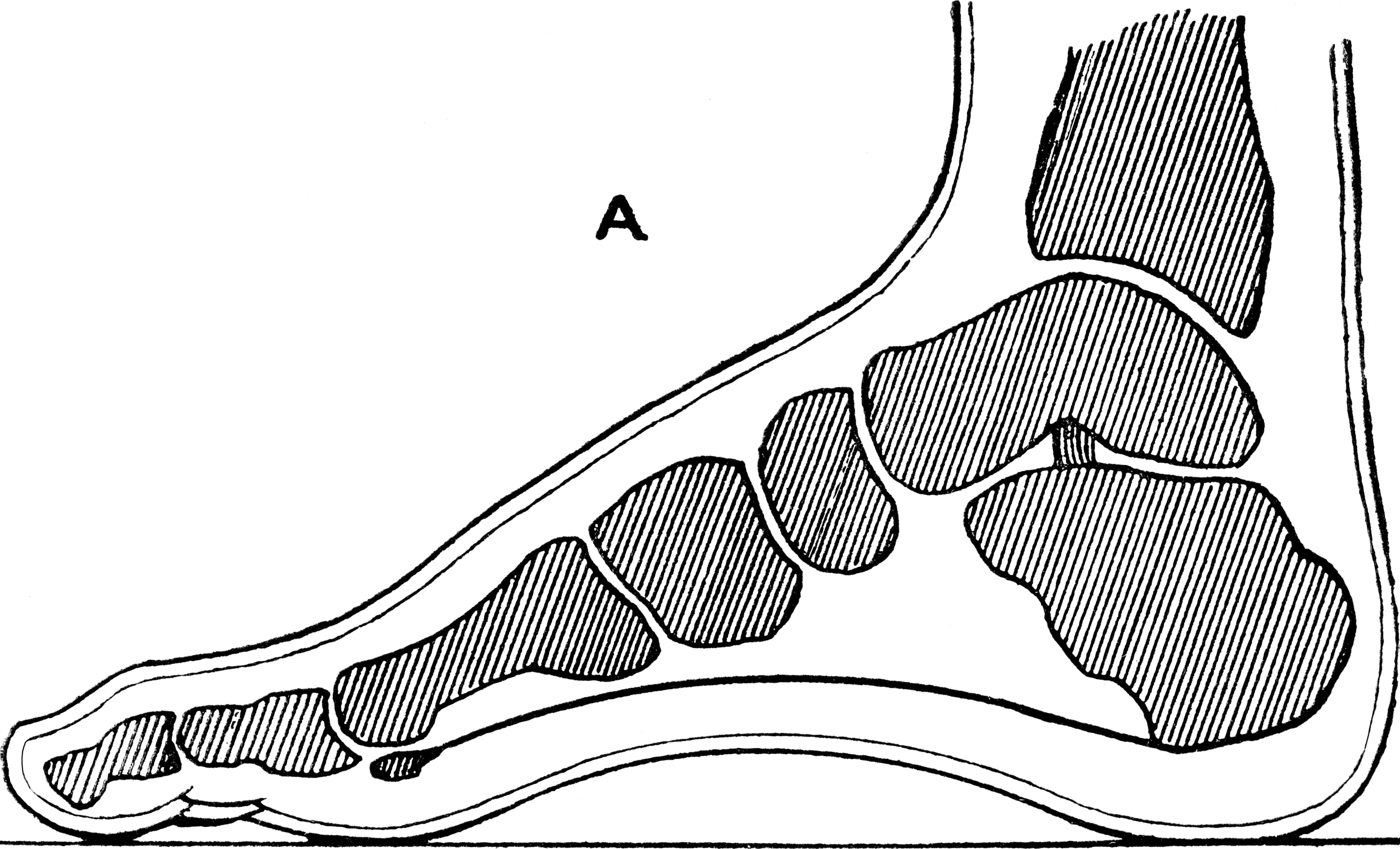
Adult Aquired Flat Foot Cause
Overview Adult-acquired flatfoot is a challenging condition to treat. It is defined as a symptomatic, progressive deformity of the foot caused by loss of supportive structures of the medial arch. It is becoming increasingly frequent with the aging population and the obesity epidemic. Patients commonly try to lose weight by exercising to improve the condition. This often leads to worsening of symptoms and progression of the disorder. Early recognition of this complex disorder is essential, if chronic pain and surgery are to be avoided. 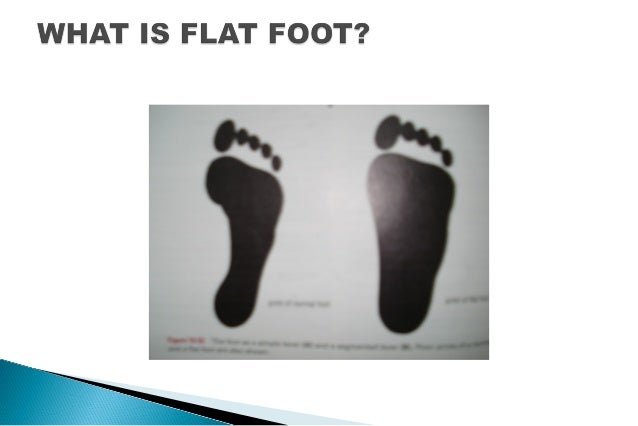 Causes Flat footedness, most people who develop the condition already have flat feet. With overuse or continuous loading, a change occurs where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Inadequate support from footwear may occasionally be a contributing factor. Trauma or injury, occasionally this condition may be due to fracture, sprain or direct blow to the tendon. Age, the risk of developing Posterior Tibial Tendon Dysfunction increases with age and research has suggested that middle aged women are more commonly affected. Other possible contributing factors - being overweight and inflammatory arthritis. Symptoms As different types of flatfoot have different causes, the associated symptoms can be different for different people. Some generalized symptoms are listed. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running and jumping, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time and may experience pain at the inside of the ankle and in the arch of the foot. Feeling like one is ?dragging their foot.? When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain in the bones and tendons in the outside of the ankle joint. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoe wear very difficult. Sometimes, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetic patients may not experience pain if they have damage to their nerves. They may only notice swelling or a large bump on the bottom of the foot. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoe wear is not used. Diagnosis Examination by your foot and ankle specialist can confirm the diagnosis for most patients. An ultrasound exam performed in the office setting can evaluate the status of the posterior tibial tendon, the tendon which is primarily responsible for supporting the arch structure of the foot. Non surgical Treatment Nonoperative therapy for adult-acquired flatfoot is a reasonable treatment option that is likely to be beneficial for most patients. In this article, we describe the results of a retrospective cohort study that focused on nonoperative measures, including bracing, physical therapy, and anti-inflammatory medications, used to treat adult-acquired flatfoot in 64 consecutive patients. The results revealed the incidence of successful nonsurgical treatment to be 87.5% (56 of 64 patients), over the 27-month observation period. Overall, 78.12% of the patients with adult-acquired flatfoot were obese (body mass index [BMI] = 30), and 62.5% of the patients who failed nonsurgical therapy were obese; however, logistic regression failed to show that BMI was statistically significantly associated with the outcome of treatment. The use of any form of bracing was statistically significantly associated with successful nonsurgical treatment (fully adjusted OR = 19.8621, 95% CI 1.8774 to 210.134), whereas the presence of a split-tear of the tibialis posterior on magnetic resonance image scans was statistically significantly associated with failed nonsurgical treatment (fully adjusted OR = 0.016, 95% CI 0.0011 to 0.2347). The results of this investigation indicate that a systematic nonsurgical treatment approach to the treatment of the adult-acquired flatfoot deformity can be successful in most cases.
Causes Flat footedness, most people who develop the condition already have flat feet. With overuse or continuous loading, a change occurs where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Inadequate support from footwear may occasionally be a contributing factor. Trauma or injury, occasionally this condition may be due to fracture, sprain or direct blow to the tendon. Age, the risk of developing Posterior Tibial Tendon Dysfunction increases with age and research has suggested that middle aged women are more commonly affected. Other possible contributing factors - being overweight and inflammatory arthritis. Symptoms As different types of flatfoot have different causes, the associated symptoms can be different for different people. Some generalized symptoms are listed. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running and jumping, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time and may experience pain at the inside of the ankle and in the arch of the foot. Feeling like one is ?dragging their foot.? When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain in the bones and tendons in the outside of the ankle joint. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoe wear very difficult. Sometimes, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetic patients may not experience pain if they have damage to their nerves. They may only notice swelling or a large bump on the bottom of the foot. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoe wear is not used. Diagnosis Examination by your foot and ankle specialist can confirm the diagnosis for most patients. An ultrasound exam performed in the office setting can evaluate the status of the posterior tibial tendon, the tendon which is primarily responsible for supporting the arch structure of the foot. Non surgical Treatment Nonoperative therapy for adult-acquired flatfoot is a reasonable treatment option that is likely to be beneficial for most patients. In this article, we describe the results of a retrospective cohort study that focused on nonoperative measures, including bracing, physical therapy, and anti-inflammatory medications, used to treat adult-acquired flatfoot in 64 consecutive patients. The results revealed the incidence of successful nonsurgical treatment to be 87.5% (56 of 64 patients), over the 27-month observation period. Overall, 78.12% of the patients with adult-acquired flatfoot were obese (body mass index [BMI] = 30), and 62.5% of the patients who failed nonsurgical therapy were obese; however, logistic regression failed to show that BMI was statistically significantly associated with the outcome of treatment. The use of any form of bracing was statistically significantly associated with successful nonsurgical treatment (fully adjusted OR = 19.8621, 95% CI 1.8774 to 210.134), whereas the presence of a split-tear of the tibialis posterior on magnetic resonance image scans was statistically significantly associated with failed nonsurgical treatment (fully adjusted OR = 0.016, 95% CI 0.0011 to 0.2347). The results of this investigation indicate that a systematic nonsurgical treatment approach to the treatment of the adult-acquired flatfoot deformity can be successful in most cases.  Surgical Treatment If surgery is necessary, a number of different procedures may be considered. The specifics of the planned surgery depend upon the stage of the disorder and the patient?s specific goals. Procedures may include ligament and muscle lengthening, removal of the inflamed tendon lining, tendon transfers, cutting and realigning bones, placement of implants to realign the foot and joint fusions. In general, early stage disease may be treated with tendon and ligament (soft-tissue) procedures with the addition of osteotomies to realign the foot. Later stage disease with either a rigidly fixed deformity or with arthritis is often treated with fusion procedures. If you are considering surgery, your doctor will speak with about the specifics of the planned procedure.
Surgical Treatment If surgery is necessary, a number of different procedures may be considered. The specifics of the planned surgery depend upon the stage of the disorder and the patient?s specific goals. Procedures may include ligament and muscle lengthening, removal of the inflamed tendon lining, tendon transfers, cutting and realigning bones, placement of implants to realign the foot and joint fusions. In general, early stage disease may be treated with tendon and ligament (soft-tissue) procedures with the addition of osteotomies to realign the foot. Later stage disease with either a rigidly fixed deformity or with arthritis is often treated with fusion procedures. If you are considering surgery, your doctor will speak with about the specifics of the planned procedure.